DOI: https://doi.org/10.1530/thienmaonline.vn-15-1164 Page(s): R117–R133 Volume/Issue: Volume 175: Issue 3
Management of Graves’ orbitopathy (GO) must be based on the correct assessment of activity and severity of the disease. Activity is usually assessed with the Clinical Activity Score, whereas severity is classified according to a European Group On Graves” Orbitopathy (EUGOGO) consensus statement as mild, moderate-to-severe, and sight-threatening. Myopathic and chronic congestive forms are uncommon clinical presentations of GO. Restoration and maintenance of stable euthyroidism are recommended in the presence of GO.
Bạn đang xem: Endocrine là gì
In moderate-to-severe disease, steroids have been widely employed and have shown to possess an anti-inflammatory activity, but about 20–30% of patients are not responsive and present recurrence. Some novel immunosuppressors have already been employed in clinical studies and have shown interesting results, although the lack of randomized and controlled trials suggests caution for their use in clinical practice. Potential targets for therapy in GO are the thyroid-stimulating hormone and the insulin-like growth factor 1 receptor on the fibroblasts, inflammatory cytokines, B and T cells, and the PIK3/mTORC1 signaling cascades for adipogenesis. A recent open study has shown that tocilizumab, an anti-sIL-6R antibody, inactivates GO. Consistent reports on the efficacy of rituximab have recently been challenged by randomized controlled trials.
As the main goal of treatment is the well-being of the patient, the therapeutic strategy should be addressed to better suit the patient needs, more than improving one or more biological parameters. The increasing availability of new therapies will expand the therapeutic options for GO patients and allow the clinician to really personalize the treatment to better suit the patients’ personal needs.
Abstract
Management of Graves’ orbitopathy (GO) must be based on the correct assessment of activity and severity of the disease. Activity is usually assessed with the Clinical Activity Score, whereas severity is classified according to a European Group On Graves” Orbitopathy (EUGOGO) consensus statement as mild, moderate-to-severe, and sight-threatening. Myopathic and chronic congestive forms are uncommon clinical presentations of GO. Restoration and maintenance of stable euthyroidism are recommended in the presence of GO.
In moderate-to-severe disease, steroids have been widely employed and have shown to possess an anti-inflammatory activity, but about 20–30% of patients are not responsive and present recurrence. Some novel immunosuppressors have already been employed in clinical studies and have shown interesting results, although the lack of randomized and controlled trials suggests caution for their use in clinical practice. Potential targets for therapy in GO are the thyroid-stimulating hormone and the insulin-like growth factor 1 receptor on the fibroblasts, inflammatory cytokines, B and T cells, and the PIK3/mTORC1 signaling cascades for adipogenesis. A recent open study has shown that tocilizumab, an anti-sIL-6R antibody, inactivates GO. Consistent reports on the efficacy of rituximab have recently been challenged by randomized controlled trials.
As the main goal of treatment is the well-being of the patient, the therapeutic strategy should be addressed to better suit the patient needs, more than improving one or more biological parameters. The increasing availability of new therapies will expand the therapeutic options for GO patients and allow the clinician to really personalize the treatment to better suit the patients’ personal needs.
Invited Author’s profile

Dr Mario Salvi was trained initially in Italy. He carried out post-doctoral research at McGill University, where he began working in the field of thyroid autoimmunity with specific focus on the pathogenesis of Graves’ disease and orbitopathy. He has been at the University of Milan since 2012. His center is a member of the EUropean Group of Graves’ Orbitopathy (EUGOGO) consortium, of which he was the Secretary from 2009 to 2015. Over the last 10 years he has developed an interest in immunotherapy for Graves’ orbitopathy and has been carrying out clinical studies with rituximab and other immunosuppressors, in addition to multicenter trials of EUGOGO. He has published more than 140 papers and has more than 180 scientific communications at international meetings.
Introduction
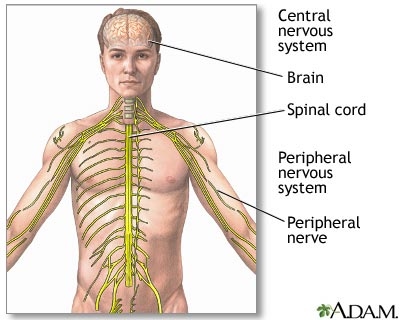
Graves’ orbitopathy (GO) is an autoimmune inflammatory disorder involving the orbital tissues. It is the most common extrathyroidal manifestation of Graves’ disease (GD) (1). Although the pathogenesis of GO is not yet clarified, immunological cross-reactivity of thyroid and orbital antigens in muscular, connective, and adipose tissues is thought to play a key role (2). Different longitudinal studies confirm that spontaneous improvement or stabilization of eye symptoms and signs may occur when GO is mild (3, 4, 5, 6, 7, 8, 9). It is well known that GO has a self-limiting natural course, characterized by a phase of active inflammation of the orbital tissues, in which disease severity generally progresses, followed by a phase of stabilization and improvement of inflammation, as described by the ‘Rundle curve’ (10, 11) (Fig. 1A). Regression of the inflammatory process may lead to fibrosis, preventing affected tissues from returning to their previous healthy, functional state. Anti-inflammatory therapy is indicated in the first phase, whereas rehabilitative surgery may be indicated in the second one (12) (Fig. 1B). Thus, management of GO must be based on the correct assessment of activity and severity of the disease. In most European clinical centers, the activity is usually assessed with the Clinical Activity Score (CAS) (13) (Table 1), whereas severity is classified according to a recent consensus statement by EUGOGO as mild, moderate-to-severe, and sight-threatening (14).
Figure 1
(A) The byphasic course of the severity of GO according to the model of Rundle (10). Dotted line shows the most severe forms of disease, generally responsive to urgent surgical decompression of the orbit. The degree of residual disease is related to successful (a) or unsuccessful (b) immunosuppression. (B) Proposed curve of the changes of activity in relation to the efficacy of immunosuppression. Shaded areas show successful (a) or unsuccessful (b) response to therapy. Persistence of chronic congestive signs may be observed even after disease inactivation. (C) Changes of quality of life (QoL) in relation to disease severity and successful (a) or unsuccessful (b) immunosuppressive therapy, based on the hypothesis that the QoL is inversely related to the degree of residual disease, as in (A).
Citation: European Journal of Endocrinology 175, 3; 10.1530/thienmaonline.vn-15-1164
3/7 or >4/10 indicates active GO.”>Table 1
Inflammatory signs of active GO. The CAS is the sum of all items present. A CAS >3/7 or >4/10 indicates active GO.
| Pain on attempted up, side, or down gaze, during the past 4 weeks | ||
| Redness of the eyelid(s) | ||
| Diffuse redness of the conjunctiva, covering at least one quadrant | ||
| Swelling of the eyelid(s) | ||
| Chemosis | ||
| Swollen caruncle | ||
| Increase of proptosis of ≥2 mm during a period of 1 –3 months | ||
| Decrease of eye movements in any direction ≥8° during a period of 1–3 months | ||
| Decrease of visual acuity of ≥1 line(s) on the Snellen chart (using a pinhole) during a period of 1–3 months | ||
| Total | 3/7 first visit | |
| 4/10 second visit |
Controversies in the diagnosis of GO
A CAS score ≥3/7 at first examination or 4/10 on follow-up visits (Table 1) qualifies the patients for a diagnosis of active GO. If the disease is of moderate-to-severe grade, the patient may benefit from the treatment with immunosuppressive therapies. There are, however, two clinical presentations of GO: a predominantly myopathic form, in which actual disease progression may not be correctly assessed with the CAS in the absence of soft tissue inflammation, and a chronic congestive form, in which soft tissue changes due to orbital congestion may be equivocally assessed as signs of active inflammation.
Myopathic GO
This form is characterized by prevalent muscle involvement resulting in motility impairment with few or absent soft tissue inflammatory signs. In patients affected with myopathic GO, diplopia often represents the first manifestation of ocular involvement and causes remarkable disability (15). To date, diplopia is qualitatively classified as absent, intermittent, inconstant or constant according to the Gorman Score (16), whereas a quantification of muscle defect may be studied by the field of binocular single vision, according to the Goldman or arc perimeter (17). A reduction of motility in any direction greater than 8°, in two subsequent ophthalmological examinations (1–3 months), is indicative of disease progression and accounts for one point of the CAS. This implies that the recent onset myopathic GO can be progressive, although inactive according to the CAS. This clinical situation is distinct from the change (usually worsening) of muscle ductions observed later during the scarring phase of GO, likely reflecting fatty degeneration and fibrosis typical of ‘inactive’ disease. In order to early identify progression in these patients with the myopathic form of GO, some authors have recently suggested to use quantitative MRI parameters, which have been shown to correlate with the changes of the CAS (18). This interesting approach, nevertheless, needs further validation before using it in daily clinical practice.
Chronic congestive GO
Congestion of the superior orbital vein plays an important role in the inflammatory phase, as demonstrated by computed tomography (19, 20, 21) and color Doppler imaging studies (22, 23, 24, 25). It has been suggested that in GO the success of the immunosuppressive treatment is the result of the effect not only on the autoimmune process but also on the reduction of orbital venous congestion. The impairment of superior orbital vein flow during the inflammatory phase of GO may otherwise persist, despite an effective outcome of immunosuppressive treatment (26). In these patients, ophthalmological signs of the persistent orbital vascular congestion may show similarities with some of those observed in active GO. Characteristic diagnostic criteria for the chronic congestive form may be eyelid edema, eyelid and conjunctival redness, chemosis, and caruncle edema associated with disease duration >12 months, orbital CT scan evidence of increased muscle and adipose tissue volume, and unresponsiveness to immnosuppressive therapy (26).
If not properly recognized, the myopathic and chronic congestive forms of GO may bring about inadequate treatments, from either a too long ‘wait-and-see’ approach in the former group of patients or an unnecessary therapy in the latter. Disease duration is perhaps the most useful parameter for the differential diagnosis of these two particular subgroups of GO patients; as previously reported by Terwee and colleagues, GO duration >16 months was a significant predictor of no change and no response to therapy (27). A very recent study has shown that the increase of fibroadipose tissue is observed in untreated patients with a longer duration of disease (28), resulting in increasing proptosis and orbital fat volume mimicking disease progression. At the first clinical examination of a patient, it is very important to precisely assess the onset of the first symptoms and the diagnosis of disease, as this can provide essential contribution to the classification of GO. Indeed, the recent onset of diplopia in a purely myopathic form allows to hypothesize progressive GO. However, the presence of signs of orbital vascular congestion in a disease of long duration, perhaps in patients with previous immunosuppressive treatment, would be suggestive of chronic congestive disease. Once the diagnosis of inactive disease is made, surgery, orbital decompression and squint surgery are the only effective treatments to improve both congestive signs, by increasing the venous outflow of the orbit, and orthotropic vision (29).
Current guidelines for treatment of thyroid dysfunction in patients with GO
Prompt restoration and maintenance of stable euthyroidism are recommended in the presence of GO, because both hyperthyroidism and hypothyroidism have a negative impact on GO (30, 31). The optimal treatment of hyperthyroidism when GO is present is, however, a challenging dilemma (32). Table 2 summarizes the current evidence from the literature. Antithyroid drugs per se do not appear to negatively affect GO once euthyroidism has been restored. This is suggested by two prospective studies in which most patients during antithyroid drug treatment had stable GO (9, 33), with only a few cases of progression or improvement compatible with the natural history of the disease. GO may improve with thyonamides only as a consequence of the restoration of euthyroidism (31) and the reduction of serum levels of thyroid-stimulating hormone (TSH) receptor (TSHR) antibodies (34). In addition, whichever regimen of antithyroid drug administration (titration vs block and replace) is employed, no difference on the GO outcome is observed.
Table 2Effect of treatments for Graves’ hyperthyroidism on GO.
| No impact on natural history of GO of antithyroid drugs | (30, 31, 32, 33, 34, 35) |
| Uncertain effect of thyroidectomy on progression of GO | (34, 35, 36) |
| De novo occurrence or progression of GO after RAI treatment with or without steroid prophylaxis | (39, 40, 41, 42, 43) |
| Postablation hypothyroidism induces progression of GO | (44, 45) |
| Stabilization of GO after total thyroid ablation (thyroidectomy followed by RAI treatment) | (46, 47, 48, 49, 50) |
Thyroidectomy, in particular near-total thyroidectomy, has been reported to be an effective treatment for hyperthyroidism (35). Scant literature exists on the effects of surgery on the course of GO, due to the difficulty in enrolling patients in studies in which surgery is planned to be the first-line therapy. One randomized clinical trial showed that the rate of de novo occurrence or progression of GO among patients submitted to thyroidectomy or medical therapy was similar but significantly lower than that observed after radioiodine (RAI) treatment (36).
RAI is an effective treatment for hyperthyroidism and represents the first-line treatment of hyperthyroidism in North America (35, 37). The majority of patients develop hypothyroidism within 1 year from RAI administration (38), although hypothyroidism may occur earlier, in some patients even 1 month after treatment. Although antithyroid drugs and thyroidectomy do not seem to affect the natural course of GO (36, 39), RAI treatment has been shown to be associated with worsening, or de novo occurrence, of GO in 5–15% of patients, mostly smokers (39, 40, 41). As 1989, it has been proposed that a short course of systemic corticosteroid treatment may prevent RAI-induced exacerbation of GO. Steroid prophylaxis has been carried out using very low doses of prednisone (0.2mg/kg body weight), given 1 day after RAI therapy, and gradually tapered down and withdrawn after 6 weeks, which has been shown to be effective in a study in Italy (42) but not in a recent study on Japanese patients (43). Alternatively, methylprednisolone can be administered intravenously at the dose of 500mg weekly for 2 weeks followed by another two weekly infusions of 250mg (cumulative dose of 1.5g) (40). The onset of hypothyroidism should be promptly assessed and corrected, because late correction of post-RAI hypothyroidism has been shown to represent a relevant risk factor for reactivation or de novo occurrence of GO (44, 45). Finally, RAI can also be administered after surgery to attain total ablation of thyroid tissue, which might be beneficial for its complete removing of thyroid antigen(s) and autoreactive T lymphocytes likely involved in the pathogenesis of GO (1). Indeed, few studies have suggested that total thyroid ablation is more frequently associated with GO improvement than surgery alone (46, 47, 48, 49, 50). According to the recently published Italian guidelines on the treatment of hyperthyroidism in patients affected with GD and GO (51), total thyroid ablation may be suggested when trying to achieve earlier inactivation of GO that can be followed, when needed, by prompt rehabilitative surgery.
The optimal therapeutical approach for thyroid dysfunction in patients with GO remains a dilemma, and decisions in most cases still rely on expert endocrinologists’ opinion, based on the age of patient, the degree of eye involvement, and, last but not least, the patients’ expectations.
Treatment of moderate-to-severe orbitopathy
Immunosuppressive therapies exert their beneficial effects only in the active phase of GO, but not in the burnout disease where only rehabilitative surgery may improve the patient’s eye appearance and function. In active progressive disease, medical treatment (immunosuppressive and/or anti-inflammatory) has the objective to reduce inflammation of eye muscles and orbital fibroadipose tissue, which may eventually reduce the need for significant subsequent rehabilitative surgery (52). According to a EUGOGO consensus paper, patients classified with moderate-to-severe GO usually have one or more of the following clinical signs: lid retraction ≥2mm, moderate or severe soft tissue involvement, exophthalmos ≥3mm above normal for race and gender, or inconstant or constant diplopia (52).
Glucocorticoids
High-dose systemic glucocorticoids (GCs) are currently the first-line treatment of active moderate-to-severe GO (3, 52, 53). Several randomized clinical trials found a response rate of approximately 70–80% in patients treated intravenously and approximately 50–60% in those treated orally (53, 54). In vitro studies have shown that GCs decrease the production of glycosaminoglycans by orbital fibroblasts, downregulate some cytokine and antibody secretion, modulate T- and B-cell functions, and decrease trafficking of neutrophils and macrophages at the inflammation sites (14, 55) (Fig. 2). Treatment effectiveness much depends on interindividual variability, but this does not seem to be related to polymorphisms of the GC receptor (56).
Figure 2
Potential targets for immunomodulatory treatments in active moderate-to-severe GO.
Citation: European Journal of Endocrinology 175, 3; 10.1530/thienmaonline.vn-15-1164
Intravenous pulsed methylprednisolone is more effective (14, 46, 57, 61) and has a better safety profile compared with oral prednisone (60, 61, 62, 63, 64, 65). Different treatment schedules have been used, with cumulative doses ranging from 4.5 to 12g and occasionally associated with oral GC interpulse or at the end of the protocol (3, 14, 54, 55, 56, 57, 58, 59). A recent multicenter randomized EUGOGO study has shown that a cumulative dose of 7.5g of methylprednisolone is more effective than intermediate or lower doses (5 or 2.25g respectively), although it is associated with more frequent adverse events (65). In particular, the high-dose regimen has a more significant and positive impact on eye muscle motility compared with lower doses. Therefore, a high-dose regimen may be used in more severe cases of GO, whereas an intermediate dose (5g) regimen is recommended when patients have more moderate disease. In a recent paper, Vannucchi et al. (56) observed that in up to 70% of patients, GO becomes inactive after the first 6–8 weeks of intravenous GC treatment, without subsequent disease relapse. These findings suggest that in these patients, steroids may be tapered off more rapidly with equal efficacy and better tolerability, compared with a full course of therapy. When deciding for therapy with intravenous methylprednisolone, a total cumulative dose of 8g should not be exceeded. Morbidity and mortality of GC therapy in GO patients have been estimated to 6.5 and 0.6% respectively (63). Acute liver failure and cardiovascular events associated with GC administration may be fatal (56, 66, 67, 68, 69, 70). A marked increase of liver enzymes, often asymptomatic, is the most common adverse observed (71) and may be caused by a direct, dose-related toxic effect of intravenous methylprenisolone (IVMP) on hepatocytes. Preexistent viral hepatitis may be a risk factor for liver damage, whereas data on coexistent liver steatosis or diabetes are conflicting (67, 68). Autoimmune hepatitis may also occur during IVMP treatment (67, 68). Screening for virus markers and autoantibodies and clinical monitoring is suggested when deciding for high-dose IVMP therapy, in order to prevent complications (64). The concurrent use of statins has been shown to potentially induce liver damage in patients undergoing intravenous GC therapy for GO (72). Therefore, we suggest to consider temporary withdrawal of these medications at the time of steroid therapy, if the patient’s clinical situation allows.
The major limitation of GC therapy is that 20–30% of patients are poorly responsive or unresponsive at all and that approximately 10–20% of patients present with disease relapse after drug withdrawal (65). A recent retrospective study has shown that responsive patients usually have inactivation of GO as early as 6–8 weeks from the beginning of GC therapy, whereas those who do not respond may be otherwise switched to other immunosuppressive treatments, alone or in combination with steroids (56).
What to do if GCs fail and moderate-to-severe GO is still active?
The management of patients in whom intravenous GC therapy gives only partial or inadequate response or of those with disease recurrence is a major challenge (57). There is no definitive agreement on how to treat these patients and the decision about a second-line treatment of active moderate-to-severe GO is based more on experts’ opinion than on clinical evidence, due to the limited studies in the literature. First, such patients ought to be referred to specialized centers, because they are more prone to develop complications. Secondly, steroids may be administered in combination with other therapies, subsequently to their initial failure as monotherapy.
Combination therapy of oral GC and orbital radiotherapy could be considered an alternative, especially in the presence of muscle involvement and diplopia, and the two therapies have been shown to have synergistic effects (73, 74). Orbital radiotherapy has been shown in randomized clinical trials to be effective in improving diplopia (75, 76), with the exception of one randomized trial that has questioned its efficacy (77). In general, the administered dose is 20 Gray (Gy) per orbit fractionated in 10 daily doses over 2 weeks (78), but also 1Gy per week over a 20-week period was shown to be equally effective and better tolerated (79). Irradiation therapy may induce mild and transient exacerbation of ocular inflammation that can be controlled by the concomitant administration of low-dose GCs (3, 80), whereas reports on long-term safety have been reassuring (81, 82). To date, there has been no evidence that intravenous GCs associated with orbital radiotherapy is more effective than steroids alone, but this interesting hypothesis will be challenged in a randomized multicenter clinical trial conducted among EUGOGO centers.
Oral GCs (starting dose, 0.5mg/kg body weight of prednisone) have also been administered in combination with cyclosporine (5mg/kg body weight) for 3 months (83, 84) to follow the initial intravenous GC treatment. Combined treatment with cyclosporine has been shown to allow reduction of GC doses and improvement of efficacy by maintaining therapy for a longer time.
These combined modalities of treatment imply retreatment with GC, a solution that may be proposed to patients with disease relapse, but hardly to nonresponders to initial GC therapy. Furthermore, in patients with more severe GO undergoing a high-dose intravenous GC regimen with a total cumulative dose of GC of 7.5g, safety concerns would prevent the clinician to plan for more steroids even if the patient had disease relapse after a significant therapeutic response to the initial GC treatment. It is also worth considering that some patients may elect not to repeat a GC-based regimen if they experienced a poor outcome with the first one. Are there real alternatives to immunosuppression with steroids in GO?
Novel targeted therapeutic modalities
Over the past decade, a series of studies have partly uncovered the mechanisms involved in GO pathogenesis, in particular those leading to cytokine-driven inflammation and increased retro-orbital adipogenesis. Based on these findings, evidence has emerged for treating progressive GO by directly targeting the specific reactions of immune and inflammatory processes that result in orbital tissue expansion and remodeling occurring in GO.
The potential property of novel immunomodulating agents is a disease-modifying and not just an anti-inflammatory effect (85). Figure 2 shows the antigens that may be specifically targeted in GO, the TSHR, the insulin-like growth factor 1 (IGF-1) receptor (IGF-1R), and the platelet-derived growth factor (PDGF) receptor, expressed on the fibroblasts, several cytokines that have been shown to be involved in disease progression and molecules regulating the immune function of antigen presentation, such as B and T cells (Fig. 2).
Most of these compounds are not yet available for clinical use in GO, and only a few of those have been employed in human studies and have shown to be potentially useful for treating patients. We will mainly focus on findings from clinical studies, which in most cases are open label studies with only few randomized controlled studies.
Xem thêm: Maintain Là Gì – định Nghĩa, Ví Dụ, Giải Thích
Low-molecular-weight TSHR ligands
Interestingly, low-molecular-weight TSHR ligands have been synthesized over the past few years. They interact with the TSHR as (i) TSHR agonists (that activate receptors), (ii) neutral antagonists (that inhibit receptor activation by agonists), and (iii) inverse agonists (that inhibit receptor activation by agonists and possess constitutive signaling). These molecules are studied for potential treatment of both GD and GO but have been tested so far only in vitro on thyrocytes (86) and orbital fibroblasts (87) (Fig. 2).
Targeting the IGF-1R
The IGF-1R was shown to be coexpressed with the TSHR on orbital fibroblasts and fibrocytes (88), and in vitro blocking of the IGF-1R attenuates TSH-dependent signaling (89). Serum IGF-1R autoantibodies have been detected only in subgroups of patients with GO (90) and do not seem to occur with significant prevalence in active GO. A phase-II multicenter, placebo-controlled randomized clinical trial, conducted in the US and in Europe (91), is currently investigating a specific human monoclonal antibody that binds to the extracellular subunit domain of IGF-1R (Teprotumumab, RV 001, R1507). Binding of Teprotumumab to IGF-1R on fibrocytes was shown to attenuate TSH-dependent interleukin (IL)-6 and IL-8 expression and Akt phosphorylation (89) (Fig. 2). The ongoing study will hopefully provide the background for potential use in current clinical practice.
Modifiers of orbital tissue remodeling
Inhibitors of PIK3/mTORC1 cascades have been shown in an in vitro model of GO to reduce hyaluronan accumulation and adipogenesis (92). Although trials with first-generation inhibitors, such as wortmannin, LY294002, or rapamycin and its derivatives, have been stopped because of significant untoward effects, second-generation inhibitors are currently being used in clinical trials on patients with refractory cancers (93), but to date, no trials have been planned in autoimmune thyroid disease.
A PDGF-BB isoform of the PDGF receptor has recently been found expressed and increased in the orbital tissue of GO patients (94, 95, 96, 97). Its signaling on orbital fibroblast can be blocked by tyrosine kinase inhibitors, such as imatinib mesylate, nilotinib ,and dasatinib, which has been shown to decrease in vitro the mRNA expression of hyaluronic synthetase 2 and IL-6 and IL-8 cytokines in orbital tissue from active GO (96) (Fig. 2). These compounds are invariably associated with serious side effects, and this may impact on their further development as effectively available therapeutic agents for GO.
Targeting cytokines/chemokines with monoclonal antibodies
The active phase of GO is driven by proinflammatory and Th1-derived cytokines, such as IL-6 and IL-1, and IFN-gamma-induced chemokines, such as CXCL10, whereas Th2-derived cytokines, including IL-4, IL-5, and IL-10, prevail in the disease inactive phase (98).
TSHR antibodies have been shown to increase the expression of IL-1 receptor on orbital fibroblasts (99) synergistically with a smoke extract (100). Anakinra, an IL-1 receptor antagonist, may antagonize this mechanism, although this hypothesis has not been challenged in a clinical trial.
Most TNF inhibitors (etanercept, infliximab, adalimumab) have been widely and successfully used in autoimmune rheumatic diseases. Etanercept, a recombinant fusion protein of extracellular ligand-binding portion of the human TNF receptor, binds TNF and blocks the interaction with its receptors, thus preventing inflammatory responses. A small trial with etanercept was conducted on ten patients with active moderate-to-severe GO in 2005 by Paridaens et al. (101) resulting in improvement of soft tissue inflammatory signs in six patients, but no advantage over therapy with GC, in terms of overall efficacy and side effects.
Activation of the IL-6/sIL-6R system has been shown in active GO by Salvi and colleagues (102). An IL-6 receptor antagonist, tocilizumab has been successfully employed in rheumatic disease (103) and recently in an open clinical trial on 18 patients with GO refractory to GC treatment (104). Disease activity improved in all patients, proptosis values decreased in 72%, and ocular motility improved in 83%. One patient who had acute optic neuropathy was able to avoid orbital decompression. Currently, a placebo-controlled trial is testing the efficacy and safety of tocilizumab in patients with moderate-to-severe or sight-threatening GO, who did not respond to treatment with pulse steroids (phase III clinical trial, randomized, placebo-controlled, double-blind, parallel groups and multicenter study, EUDRACT 2010-023841-31). The results of this study are expected in the Spring of 2016.
The detection of increased serum BAFF concentrations in patients with either Hashimoto’s thyroiditis (105) or GD, with and without orbitopathy (106), suggests that targeting BAFF may be an option in the management of GD. The therapeutic efficacy of belimumab, a monoclonal antibody against BAFF, has been challenged so far in patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) with moderate clinical benefits, mostly in SLE. A randomized controlled trial of belimumab compared with intravenous steroids in active GO will start at the beginning of 2016 (EUDRACT 2015-002127-26). This treatment might affect the secretion of TSHR autoantibodies as well as the B-cell-driven immune mechanisms involved with GO (Fig. 2).
Rituximab
Following the first report on a successful treatment of one patient with moderate-to-severe GO (107), several noncontrolled studies on the effects of rituximab (RTX) in GO have appeared in the literature (108). More recently, two randomized controlled trials in moderate-to-severe GO comparing RTX with placebo (109) and to steroids (110), respectively, have just been published. Although these trials provide conflicting results, most nonrandomized studies suggested that RTX might be beneficial for moderate-to-severe and active GO (110).
RTX is a mouse–human monoclonal antibody that targets CD20. This is a human B-lymphocyte-specific antigen is expressed on B cells in the various stages of maturation, but not on plasma cells (111). To date, it has been approved for clinical use in rheumatoid arthritis and antineutrophil cytoplasmic antibody-associated vasculitis. The rationale for using RTX in GO is the potential blockade of the generation of TSHR antibodies and of inflammatory cytokines. RTX may also block B-cell antigen presentation fairly rapidly upon depletion (112), but not the interaction between B and T cells, without therefore producing an effect on specific pathogenic autoantibodies (113) (Fig. 2).
To date, clinical studies have shown that RTX can be employed in patients with active moderate-to-severe GO either as first-line treatment or when IVMP therapy fails (114, 115, 116, 117, 118, 119).
Efficacy and dosing of RTX in GO
In earlier reports (107, 114), RTX has been employed in patients with active steroid-resistant GO. In an open study, RTX has subsequently been used as a first-line therapy in previously untreated patients (115). Disease inactivation at 24 weeks and lack of disease relapse up to 18 months of follow-up were observed, whereas GO is generally reported to relapse in 10–20% of patients after IVMP (65).
More recently, two randomized clinical trials have studied the efficacy of RTX in patients with active moderate-to-severe GO. Salvi et al. (110) have randomized 32 patients with either RTX or IVMP and studied the decrease of the CAS as a primary end point at 24 weeks. The CAS improved in 100% of patients after RTX compared with 69% after IVMP (P109) were not able to find RTX effective in treating active GO, compared with placebo. The study included 21 patients, of whom two developed optic neuropathy. Reasons for the conflicting results of these two studies are unknown, but differences in the patients’ population included may have had an important impact on the treatment outcomes. A much longer GO duration (11.2 vs 4.5 months) in the trial of Stan et al. (109) may have resulted in treating patients with more congestive than active, inflammatory disease. A greater number of patients previously treated with steroids (40 vs 19%) and a lesser degree of motility involvement (mean diplopia score 2 vs 3.5) was infact included in their study. Failure of RTX treatment and subsequent progression to acute DON, similarly to the two patients herein described, was previously reported (120). One possible explanation is that subclinical DON was already present in these patients at the time of therapy and that the release of cytokines induced by RTX might have resulted in increased intraorbital edema with optic nerve compression. To date, RTX has been employed in another ten patients with dysthyroid optic neuropathy (DON) (116, 118, 121) and has induced significant improvement of vision. We therefore suggest caution in employing RTX in very severe GO, particularly if subclinical DON is suspected, until randomized controlled trials will provide evidence of its superiority over standard treatment with high-dose IVMP.
Optimal dosing schedules of RTX in GO are undetermined due to the lack of randomized trials. The infusion of 1000mg twice, with a 2-week interval, has been employed as the standard treatment of RA and other autoimmune diseases. This dose has been initially used in most open studies (115, 118) and in case reports (107, 114) in patients with GO. Rapid and complete peripheral B-cell depletion following very low-dose (100mg) RTX was shown in a study by Salvi et al. (112). These patients presented a rapidly occurring orbital tissue edema that spontaneously resolved within 60–90 min. Interestingly, these patients had complete GO inactivation within a few weeks, and therefore were cured with an RTX dose about 20 times lower than the standard dose suggested in systemic autoimmune disease. In addition, a dose finding analysis in the clinical trial of Salvi et al. (110) has shown the efficacy of a single 500mg RTX dose compared with two doses of 1000mg.
Side effects of RTX
Studies addressing dose–response relationship in relation to its potential impact on the safety of RTX therapy are lacking. A recent meta-analysis of randomized studies has shown no significant differences in the primary clinical outcomes in RA when 1000mg twice were compared with 500mg twice, 2 weeks apart (122). Lower RTX doses also imply a significant reduction of treatment costs in chronic disease and the incidence of the initial infusion reactions, commonly described due to the chimeric nature of RTX. These reactions may be present in 10–30% of patients at first infusion and can be severe, but reversible (123). The underlying mechanism is the release of proinflammatory cytokines from macrophages, monocytes, lymphocytes, and NK cells. Infections have been reported as a major side effect mostly due to the hypogammaglobulinemia resulting from repeated RTX doses, although in recent large retrospective studies in patients with multiple autoimmunity severe infections were more frequently associated with treatment with steroids and other immunosuppressive agents than to hypogammaglobulinemia (124). The rare occurrence of progressive multifocal leukoencephalopathy has been reported in patients after RTX, although all of these patients had previously been treated with other immunosuppressive therapies, including cyclophosphamide, azathioprine, and even steroids, oral prednisone, or intravenous steroids (125).
Treatment of sight-threatening ophthalmopathy
Sight-threatening GO, known also as DON, is due to either compressive optic neuropathy, caused by severe hypertrophy of eye muscles at the orbital apex, or severe corneal damage resulting from severe corneal exposure, caused by excessive proptosis of the ocular globe and severe orbital congestion. In general, DON accounts for about 3–5% of all cases of GO and cigarette smoking, the male gender, restrictive strabismus, and rapidly progressive GO are considered risk factors for its development (73, 126). The diagnosis of DON is often challenging, in particular in more subclinical forms in which the progression to overt forms is not always straightforward. A survey among EUGOGO members in 2007 found that optic disc swelling, impaired color vision, and CT scan evidence of apical crowding, with potential compression optic nerve, are the most useful predictive features (126). When present, optic disc swelling is very specific for DON, but patients may also have normal appearance of optic nerve due to the combination of edema and optic nerve atrophy.
The standard therapy for DON is urgent surgical orbital decompression, although a few studies have shown that as many as 40% of patients may respond to a course of high-dose IVMP within 1–2 weeks from the initial signs of visual deterioration (127, 128). The first-line treatment of DON should be a cycle of high-dose IVMP, either 500 or 1000mg daily for three consecutive days, repeated 1 week later. An accurate clinical ophthalmological examination at 2 weeks is required to assess response and recovery of normal vision. At that point, this therapy may be continued with weekly IVMP pulses, up to a cumulative dose of 8g, if GO is still in the active phase (127, 128). Some patients improve slowly, and the extent to which a full recovery of optic nerve function is attained is currently not known. Urgent orbital decompression is mandatory if patients do not respond to IVMP or when such treatment is contraindicated (125, 126).
Outcome of treatment and patient”s satisfaction
GO has great influence on the QoL of affected patients, especially those with some degree of functional impairment such as diplopia or oppressive pain due to chronic orbital congestion. In particular, double vision severely affects the patients’ QoL, as they experience difficulties in reading, driving, and daily working activities.
Medical treatments (immunosuppressive/anti-inflammatory) are beneficial only in the active phase of the disease with the objective to decrease inflammation and reduce progression of disease severity and, consequently, the need for subsequent rehabilitative surgery. The main goal of corrective surgery is to improve visual function, preserve the cornea, and reduce the eyelid retraction and the orbital congestion resulting from the expansion of the orbital content associated with GO. The optimal surgical treatment should be tailored to the patient-specific needs, in particular to the reduction of the degree of residual disease, to the anatomical characteristics of the orbit, and to the impact of GO on the patients’ QoL.
De novo occurrence or worsening of diplopia is the most frequent complication of orbital decompression, particularly when the orbital floor is removed (129, 130). The overall prevalence of postoperative diplopia in primary gaze is around 20% (131, 132) and may require additional surgery for strabismus. The aim of eye muscle surgery is to align the eyes and to restore single binocular vision in primary and reading positions. In order to achieve this goal, multiple operations may be necessary. However, the persistence of diplopia in extreme upgaze is common, but it is usually well tolerated with a negligible effect on overall visual function (133). Eyelid surgery is generally the last step of rehabilitation, and its aim is the correction of residual eyelid malpositions after medical treatment or orbital decompression (133).
According to a recent survey, the satisfaction of GO patients with therapy is often insufficient. It has been estimated that about 30% of patients attending a thyroid–eye clinic and nearly the half of those attending a nonspecialist clinic, are not fully satisfied with the treatments they have received. This suggests first that the late referral of patients to a joint thyroid–eye clinic may positively affect the final outcome of the disease (134), and secondly, that although medical and surgical techniques have improved over time, GO still has a marked negative effect on the patients’ QoL even many years after treatment and that should be considered a chronic disease (135). This is probably due to the fact that the face is the seat of recognition for a human being, and living with a change in the appearance, as a result of any pathological condition, is always a challenging task (136).
Measurement of QoL in GO
The concept of QoL encompasses different aspects of physical and mental health, including health risks, functional status, social support, and socioeconomic status (137, 138, 139). For this reason, the quantification of QoL has become increasingly important in health care. The most common strategy for measuring the QoL consists in the administration of questionnaires or interviews, which investigate the patient’s personal feeling about the disease or the therapy (140). A disease-specific questionnaire (GO-QoL) was developed by Terwee et al. in 1998 (141) and was the first instrument designed specifically to measure health related (HR)-QoL in patients with GO. It consists of 16 questions focusing on two specific subscales: 8 questions explore the visual impairment due to decreased visual acuity and/or diplopia; the remaining 8 questions describe the psychosocial effects of facial disfigurement. The use of GO-QoL has several advantages: first, it is simple, as the score is easy to calculate, self-administered, and reproducible (142); secondly, the GO-QoL strongly correlates with the severity of GO manifestations, and, to a lesser extent, with disease activity (140) (Fig. 1C). Thirdly, the score is a reliable measure of the disease changes over time (142) or as a consequence of a medical (143) or surgical (144) treatment. In this context, a mean change of at least 6 points on one or both subscales suggests a significant change in daily functioning. For more aggressive therapies, a change of at least 10 points is usually considered as the minimal clinically relevant difference (143). The GO-QoL has been validated in different populations (145, 146, 147, 148) and translated into 15 different languages. For these reasons, QoL has become also suitable as an outcome measure of therapeutic response in RTC trials, and an improvement of GO-QoL has been shown in patients responsive to therapy.
In patients undergoing surgical treatments, the GO-QoL score increases significantly for both visual functioning and appearance after the first strabismus surgery in GO patients, showing the highest improvement for visual functioning-related questions. No differences were found in the QoL in patients previously submitted to orbital decompression compared with those who only underwent squint surgery (144). Medical treatment yields more conflicting results. Compared with oral steroids, IVMP has been associated with a significantly higher improvement either in the visual or in psychosocial functioning (5) (Fig. 1C). Conversely, in a recent study comparing IVMP and RTC, the analysis of the GO-QoL has shown significant improvement in IVMP patients for the appearance scale, but not for the visual functioning scale, whereas RTX was associated with an improvement in both scales (110).
These conflicting results may be addressed by studying the degree of the improvement of GO-QoL also considering the different therapeutic protocols and the different degrees of orbital involvement before therapy. In addition, a statistical correction for age, gender, and sociopsychological background must also be considered. Despite these limitations, it has been suggested that the routine administration of the GO-QoL in daily clinical practice is likely to improve the quality of care and to identify patients who need further psychological support (149).
These psychological implications of GO may also be further studied by means of a more specific questionnaire. In 2005, Yeatts et al. (140) developed a questionnaire of 105 questions investigating four areas (general and mental health, self-perception and social functioning, general visual function, specific visual function) in relation to GO. They found that GO patients had a lower score for all measures of QoL compared with a control group. In particular, GO patients experience difficulties in the physical and mental components, the self-perception, and social desirability. Although the results were not age or gender specific, women appeared to have a stronger decline in self-perception compared with men. Compared with other visually impaired groups, GO patients had a score similar to those of patients with diabetic retinopathy or macular degeneration.
When measured with a questionnaire assessing general moods, such as the Medical Outcomes Study-24 (MOS-24), GO patients scored worse than controls or other groups of patients with chronic diseases as heart failure, diabetes, and emphysema (150). As depression and anxiety have been associated with GO (151), it has been suggested that psychological counseling or, when necessary, referral to a psychiatric service should be offered to GO patients (152) in order to improve the patients’ QoL. Consistently with this hypothesis, in a study on 25 GO patients (153), Estcourt et al. showed an alteration of personality as a direct consequence of the physical changes associated with GO. In particular, the occurrence of frustration and depression, the concern on the potential effects of GO on job security and career progression, and anxiety have a great impact on the patients’ coping strategies and even on the interactions with health-care professionals. Referral to a psychologist may be beneficial in selected patients, similar to what reported for other diseases causing physical disfigurement (154). However, it has been estimated that about 75% of patients with GO felt that they did not receive significant professional support for their psychological problems (153), suggesting that this issue is often overlooked by clinicians.
Xem thêm: Iatrogenic Là Gì – Iatrogenic Có Nghĩa Gì
Patients with GO are also often involved with an important and life-affecting occupational impairment. In a survey on 192 workers affected with GO, nearly 20% of patients were unfit to work for a 1 month, whereas 3% were unfit for 4–6 months (155). The main determinants of working disability and the consequent impaired earning capacity are eye muscle motility disorders, whereas proptosis does not seem to influence the occupational status. This suggests that functional impairment plays a greater role in disability than in cosmetic implications (156). The occupational impairment has significant economic consequences of public health relevance, and for this reason, preventive care and rapid rehabilitation should be offered to GO patients (155).
Chuyên mục: Hỏi Đáp